Understanding Brain Bleed (Intracranial Hemorrhage)
What Is an Intracranial Hemorrhage?
An Intracranial Hemorrhage occurs when a blood vessel ruptures inside the skull, causing blood to leak into or around the brain tissue. The accumulating blood increases pressure, deprives brain cells of oxygen, and can lead to life-threatening complications without swift medical intervention.
Our multidisciplinary neuro team combines real-time imaging, micro-surgical techniques, and comprehensive critical-care protocols to maximise recovery and minimise long-term disability.
Are brain bleeds fatal?
Brain bleeds can be fatal, especially if not treated quickly. Their seriousness depends on several key factors:
Cause & Location: Bleeds deep within the brain tissue or in critical regions like the brain stem are more dangerous.
Size of the bleed: Larger hemorrhages raise intracranial pressure sharply, compressing healthy brain tissue.
Time until treatment: Brain cells begin dying just minutes after oxygen stops. Every moment counts.
Overall health & response: Older age, uncontrolled blood pressure, and being on blood thinners all worsen outcomes.
🔍 How Dangerous Are They?
Intracerebral Hemorrhage (ICH) has a nearly 50% mortality rate within 30 days. Only about 20% of patients regain good functioning.
Subdural Hematomas (acute) are even more lethal—50% to 90% fatal depending on severity.
Subarachnoid Hemorrhage also carries high risk: around 45% die within one month, and many survivors face long-term disability.
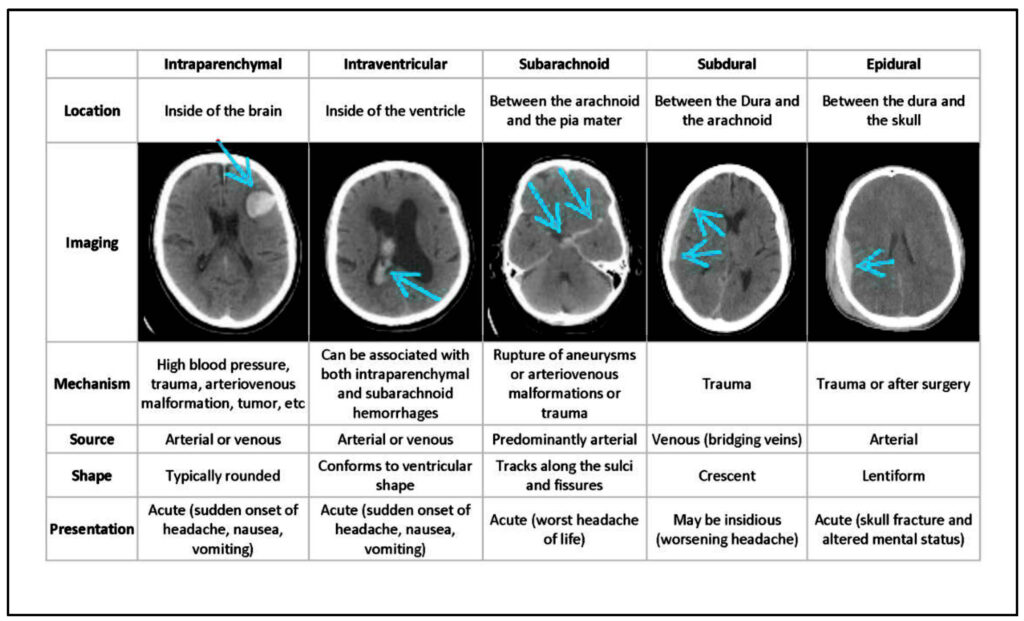
The Four Main Types (By Location)
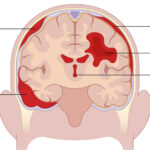
1. Bleeds Outside the Brain Tissue (Extra‑axial Hemorrhages)
These occur between the skull and the brain’s protective layers (the meninges):
• Epidural Hematoma
Blood collects between the skull and the dura mater (the tough outer membrane).
Often caused by head trauma that tears an artery (commonly the middle meningeal artery).
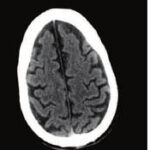
Forms a lens-shaped (biconvex) collection on CT scans
• Subdural Hematoma
Blood pools between the dura mater and the arachnoid mater.
Usually results from torn “bridging veins”—often after a head injury.
Crescent-shaped on imaging; may develop slowly in elderly or patients on blood thinners.
• Subarachnoid Hemorrhage
Blood leaks into the space between the Arachnoid and Pia Mater.
Can be due to trauma or from a ruptured cerebral aneurysm.
Presents with a sudden, severe “thunderclap” headache; visible around the brain’s sulci and cisterns on CT
2. Bleeds Within the Brain Tissue (Intra‑axial Hemorrhages)
These occur inside the brain substance itself or its fluid-filled cavities:
• Intracerebral (Intraparenchymal) Hemorrhage
Bleeding happens directly inside brain tissue—common in lobes, brainstem, or cerebellum.
Often caused by high blood pressure, vascular malformations, trauma, or tumors.
Appears as dense, irregular areas on CT scans.
• Intraventricular Hemorrhage
Bleeding enters the Ventricular system, where cerebrospinal fluid is made.
- May happen on its own (rare) or more commonly when intracerebral or subarachnoid bleeds extend into the ventricles.
 Symptoms of a Brain Bleed
Symptoms of a Brain Bleed
Most Common Early Signs
Sudden, severe headache – often described as the worst headache of one’s life, striking rapidly like a thunderclap.
One-sided weakness, numbness, or tingling in the face, arm, or leg.
Nausea and vomiting, which may appear alongside headache.
Confusion or slurred speech, indicating disrupted brain function.
Dizziness or loss of coordination, affecting balance
Sleepiness or low energy, as the brain struggles
Other Possible Symptoms
Vision problems: blurred, double vision, or partial vision loss.
Neck stiffness and sensitivity to light, especially with subarachnoid hemorrhage .
Difficulty swallowing, due to pressure on the brain-stem.
Seizures, or sudden shaking, which may herald a bleed.
Abnormal breathing or heart rate, from increased brain pressure.
Loss of consciousness or coma, occurring in severe cases .
 The Earliest Warning Sign?
The Earliest Warning Sign?
In most scenarios, the sudden onset of an intense headache is the first and most noticeable symptom.
Prompt recognition of these symptoms—especially sudden headache, one-sided weakness, or altered speech—is vital. A brain bleed is a medical emergency; immediate evaluation (such as a CT scan) and treatment can significantly improve survival chances and outcomes.
Bottom line:
If someone suddenly experiences a severe headache, any combination of weakness, confusion, vomiting, seizure, or vision loss—seek emergency medical care right away.
Complications if Treatment Is Delayed
Permanent cell loss from oxygen deprivation, causing irreversible brain damage.
Cognitive problems such as memory loss and slower thinking.
Speech and swallowing difficulties when language or brain‑stem centres are injured.
Movement and balance deficits, ranging from clumsiness to full paralysis on one side.
Sensory loss or vision loss if bleeding affects optic pathways.
Seizures triggered by irritated brain tissue
Mood or personality changes (e.g., depression, anxiety, impulsiveness) after frontal‑lobe or limbic injury.
Breathing or heart‑rate problems when pressure spreads to the brain‑stem.
Diagnosis & Tests
Urgent Neuro exam to gauge consciousness and focal deficits.
Non‑contrast CT scan: fastest way to spot fresh blood.
MRI / MRA or CT‑angiography to map hidden aneurysms or AVMs.
Extra studies (EEG for seizures, angiography, lumbar puncture, labs) to identify the cause and guide therapy.
Treatment
Surgical Options
Burr‑hole decompression or Ventricular drain to let trapped blood and pressure escape.
Decompress Craniectomy or Craniotomy/Craniectomy to remove a bone flap, evacuate clot, and repair the vessel.
Medical Management
Rapid control of blood pressure, reversal of blood thinners, seizure prevention, pain relief, and steroids for swelling when indicated.
Ventilator support, IV fluids, and careful ICU monitoring until pressure and chemistry stabilise.
Possible Side‑Effects
Surgery can lead to infection, further bleeding, or Neurologic worsening despite expert technique.
Medicines may cause drowsiness, electrolyte shifts, constipation, or blood‑pressure swings, which clinicians balance against their benefits.
Rehabilitation & Long‑Term Care
Physical therapy to rebuild strength, balance, and gait.
Occupational therapy for hand skills, dressing, and home adaptations.
Speech‑language therapy for talking, comprehension, and safe swallowing.
Lifestyle changes (blood‑pressure control, no smoking, moderation of alcohol) to lower the risk of another bleed.
Recovery time varies widely: some patients regain independence within months, while others need lifelong assistance. Early, intensive rehab offers the best odds of reclaiming lost abilities and adapting to any lasting deficits.
 In Summary
In Summary
Brain bleeds are Medical Emergencies that can cause permanent disability—or death—within hours or days. The sooner someone receives care (imaging, surgery, or medication), the better their chance at survival and recovery. Promptly calling on 76966-75086 LIFELONG NEUROCARE’s Emergency Services for Sudden Headaches, Neurological Changes, or Head Trauma is crucial—It can make the difference between life and death.